Says infectious disease doctor, allergist-immunologist
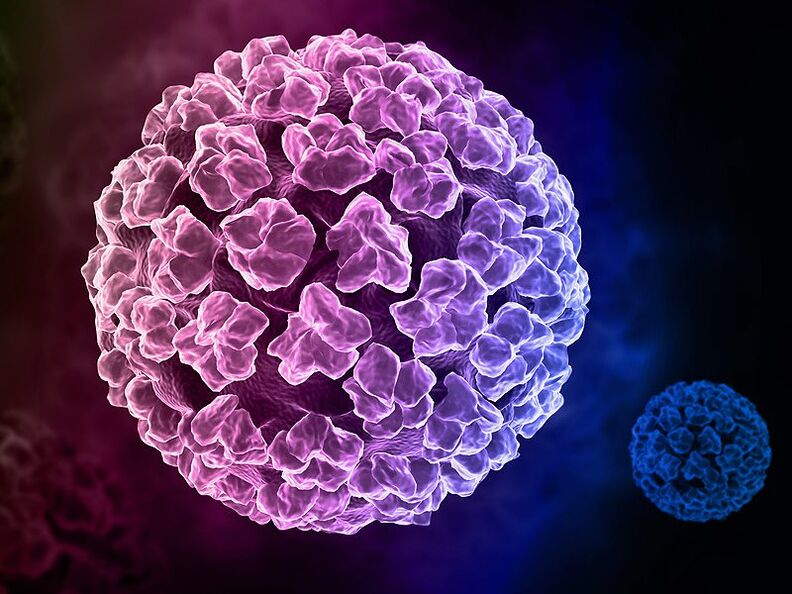
Human papillomavirus (HPV, or HPV - human papilloma virus) is a widespread virus that causes a variety of diseases in both women and men. More than half of the world's population is infected with HPV. Some of them are simply carriers of the disease, while in others this virus manifests itself as papillomatosis of the skin and mucous membranes. Approximately 30 types cause damage to the female genital organs. Sometimes this viral disease can be the causative agent of cancerous degeneration of cells. The most dangerous of them are types of papillomavirus with a high oncological risk - i. e. viruses that have the greatest ability to cause cancer of the genital organs, in particular cancer of the cervix. According to H. zur Hausen, who was awarded the Nobel Prize for research, cervical cancer is caused by 16 and 18 subtypes in 95%, and all together - in 99. 8%. Human papillomavirus is the second (after genital herpes) most common viral infection of the female genital area.
Papillomaviruses are found in about 70% of women. In addition, this benign neoplasm is formed in any area of the body:
- neck
- under the breast;
- on the stomach;
- face;
- in the armpits;
- on the mucous membranes of the mouth, nasal cavities, lips;
- on the mucous membranes of internal organs.
This infection refers to intracellular parasites that are unable to reproduce on their own, and for this they use the cells of the human body.
The transmission of the virus occurs through contact with the skin or mucous membranes of an infected person.
Infection can happen:
- during sexual intercourse (including through anal and oral types of sexual intercourse);
- at birth. From mother to newborn baby as it passes through the birth canal during childbirth. The disease is detected in the early years, when papillomas can appear in the mouth (laryngeal papillomatosis) and on the skin;
- in the absence of personal hygiene rules - when shaving or epilating;
- household way. Due to the fact that such a virus is extremely tenacious, and especially in a humid environment, there is a risk of catching it when using public places: saunas, swimming pools, toilets, baths, gyms. The virus penetrates through the smallest breaks in the skin.
Some type of virus can be contracted even by shaking hands. If there is someone in the family who is a carrier of the virus, then the risk that the rest of the family is sick with it is very high. This virus is highly contagious.
Factors contributing to HPV infection:
- decrease in general immunity due to the influence of various carcinogens;
- overwork, the presence of stress of a different nature;
- failure in the hormonal background;
- pregnancy (due to the restructuring of the body and changes in hormonal levels);
- the presence of diseases that cause disorders of metabolism and metabolism.
If the virus enters a healthy body, with good immunity, then immune cells destroy it, and infection does not occur, it does not threaten a completely healthy person.
Important! Men are more likely to act as passive carriers of the virus, which is less dangerous for men than for women - they are much less likely to develop oncology. Children under the influence of the virus may develop warts on the skin, papillomatosis of the larynx (usually in a chronic relapsing form). Papillomatosis of the larynx causes breathing problems, up to suffocation syndrome. Skin warts are present in 12% of schoolchildren, this is the most common dermatological disease in children. Remember! Regular check-ups with your doctor can help prevent the onset of cervical cancer caused by HPV. Since outwardly this disease may not manifest itself.
The following research methods are used to diagnose human papillomavirus:
- personal examination of the patient;
- blood analysis;
- colposcopy;
- smear cytology - Pap test;
- tissue histology;
PCR - polymerase chain reaction. This analysis allows not only to find out about the presence of the virus, but also to determine its type. But if the analysis is positive, this does not mean that this type of HPV will not go away on its own. This analysis also identifies all types of papillomavirus;
- ureteroscopy;
- biopsy
To detect HPV, special HPV tests are used. The most common is PCR analysis, which allows not only to identify HPV, but also to clarify its type. However, it is better to use a quantitative HPV test to assess viral load. This method allows you to determine the critical concentration of the virus, which is directly related to the risk of malignancy. Such an analysis also makes it possible to evaluate the effectiveness of the treatment, since it is not always possible to completely get rid of the virus, however, treatment can reduce its activity.
Due to the fact that HPV can be the cause of diseases of various organs, if it is present, they turn to doctors in various fields: a dermatologist, surgeon, urologist, gynecologist, proctologist, oncologist. otolaryngologist, infectious disease specialist.
So is HPV fully curable or not? To date, no antiviral drug is known that can remove HPV from the body.
One of the methods of treatment is the removal of papillomas. The main removal methods are as follows:
- surgical.
- radiosurgical.
- laser. This method is non-contact and bloodless. A crust remains at the site of removal, healing occurs under it. electrocoagulation. cryocoagulation. Complete removal of papillomas occurs after several sessions. After removal, antiviral treatment and means to restore and strengthen immunity are prescribed. Another method of preventing the disease is the HPV vaccination. Vaccination is used both as a prophylaxis and for treatment after surgery. It is carried out for boys aged 9-17 years, girls from 9 years old, women of childbearing age.
In our clinic, we use a combination of destructive methods of treatment (diathermoelectrocoagulation, radio wave coagulation or laser removal of genital warts) with the use of antiviral drugs that also affect the immune status of the patient. The advantage of our treatment regimen for HPV infections is that we not only remove warts, but also increase the body's resistance to viruses, preventing them from spreading. For each patient, we develop schemes for further management, including special anti-relapse courses of treatment.
We can promise each patient who comes to our clinic a qualitative examination (including determining the amount of the type of virus), if necessary, a special study of immune reactivity and, in any case, the selection of an individual treatment regimen, the development of an effective anti-relapse course.
One of the latest developments in the treatment of HPV INFECTION is a vaccine to prevent infection caused by HPV, which, according to scientists, should also prevent the occurrence of cervical cancer. The development of various types of HPV vaccines began in the early 1980s. Initial data formed the basis for large clinical trials in women of various age groups, as well as in children. Since then, significant progress has been made in improving vaccines, and evidence of their effectiveness and safety has been obtained. Currently, three types of vaccines have been developed.
On the territory of our country, 2 vaccines are registered: a vaccine against 4 types of HPV (16, 18, 6, 11) and a vaccine against 2 types (16, 18 types). The vaccine is intended for children from 9 years of age before the onset of sexual activity (the greatest protective effect of the vaccine) and women of childbearing age. in the latter case, protection is formed only against those types of virus that the woman did not have time to become infected with.
Vaccines are effective in preventing cervical cancer, genital warts, and cancer of the vulva and vagina. The highest clinical efficacy and safety of vaccines was confirmed by the analysis of 4 large clinical studies.
Dear friends, If you suffer from papillomatosis or have been diagnosed with the human papillomavirus, but you do not see any manifestations, or maybe you just want to make sure that you are healthy, make an appointment with an infectious disease specialist, an allergist-immunologist who specializes in the treatment of this disease. The doctor will be able to choose the best plan for the diagnosis and treatment of this disease.















